Dr Sarah Pitt
IBMS President Elect
Stronger diagnostics improve patient flow and safety in winter. Focus on people, standardised pathways and validated technology.
Winter places the NHS under intense pressure. You see the impact daily in demand, flow and difficult choices. Effective diagnostics is one of the most reliable ways to relieve that pressure, enabling earlier decisions, safer discharge and better use of clinical time.
End-to-end standardisation
Biomedical scientists and support staff keep services safe. Winter plans should protect quality as activity rises, which means maintaining training and supervision, not pausing them. It means using established scopes of practice so that advanced and consultant-level scientists can lead service improvement. Also, it means retention. Small steps help: protected time for quality tasks, access to CPD and clear routes to progress. These are not extra — they are how you sustain capacity without risking errors or repeat testing.
Turnaround times improve when processes are standardised end-to-end. Focus on the basics. Ensure good test requesting and sample quality, as well as reliable transport and tracking. Agree on clear prioritisation with clinical teams. Use data to remove variation and set realistic, shared expectations. Networked services can smooth surges if escalation pathways are known in advance. The aim is simple: the right test, first time, reported in time to change care.
Effective diagnostics is one of the most reliable ways to relieve that pressure,
enabling earlier decisions, safer discharge and better use of clinical time.
Safe technology use
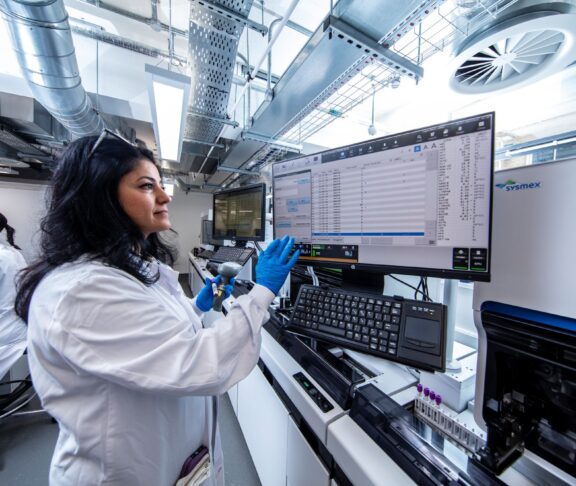
New in vitro diagnostics (IVDs), point-of-care testing (POCT) and digital tools can add capacity, but only when introduced safely. Verification, quality control and clinical interpretation remain essential. POCT needs proper governance and connectivity to the laboratory information management system (LIMS). Algorithmic decision support should be transparent and overseen by qualified staff. With these safeguards in place, technology reduces delays and supports clinicians without adding risk.
For a stronger response, involve laboratory leads in winter planning now. Agree on measurable changes for December to March. Protect time for quality and training. Remove one bottleneck in the sample flow. Prioritise one safe technology change that will stick beyond winter.
Diagnostics is a team effort across the NHS. If you involve your laboratory colleagues early, set shared goals and hold the line on quality — you will feel the benefit in wards and clinics. Patients will move faster to the right care. Staff will spend more time where they add the most value — that is winter resilience.