
Tara Spires-Jones
Professor of Neurodegeneration Deputy Director, Centre for Discovery Brain Sciences, Group Leader in the UK Dementia Research Institute
Read more at: tinyurl.com/Spires-Jones
Fundamental research at the University of Edinburgh is providing links between genes, lifestyle factors, and the brain changes that cause Alzheimer’s disease.
Age, risk genes, and lifestyle factors like obesity and smoking are associated with increased risk of developing Alzheimer’s disease. Our group is working to understand how these risk factors change the brain.
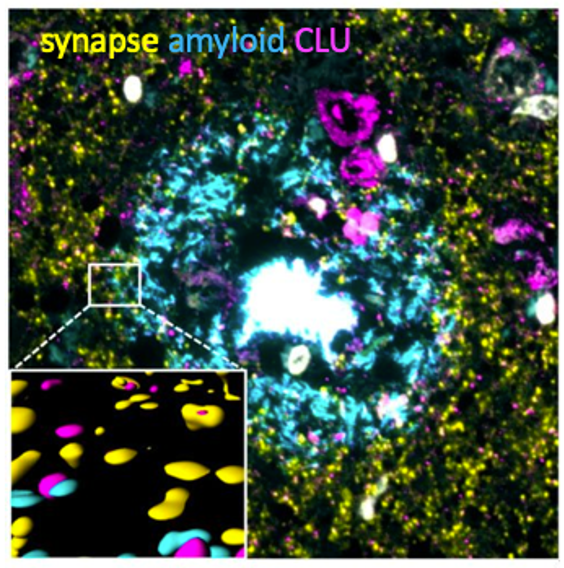
Risk genes damage synapses
Our team discovered that two of the genes that increase risk of Alzheimer’s increase, called APOE4 and CLU, cause clumping of toxic amyloid beta protein in synapses. Synapses are connections between neurons that are essential for brain function, and loss of synapses is a strong predictor of cognitive symptoms of Alzheimer’s. Our work indicates that damaging synapses is one of the ways genes can increase risk for Alzheimer’s.
Enflamed immune cells ‘eat’ synapses
Many risk genes for Alzheimer’s are not active in neurons – the cells that do the thinking – but rather in the brain immune cells called microglia. We observe that these immune cells become inflammatory and destroy synapses. In work funded by Alzheimer’s Society, we recently observed that the APOE4 gene is associated with more inflammatory changes in the brain.
These experiments suggest that another way risk genes influence the brain is through making glial cells more inflammatory, which causes them to “eat” synapses.
Lifestyle affects inflammation
Brand new data are giving us hints that lifestyle factors may also influence the brain through inflammation. Inflammatory markers in blood samples increase with age. These inflammatory changes are associated with smoking and high body mass index and also track with poorer cognitive function during ageing.
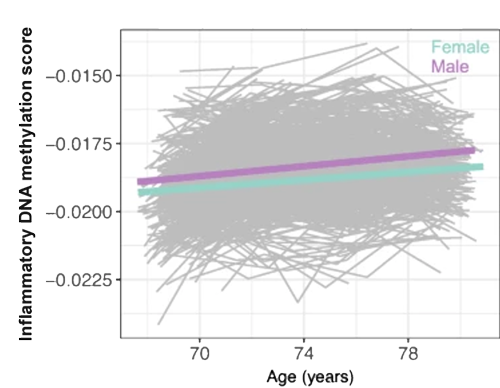
These data link lifestyle with inflammation in the body that affects brain function as people age. We are working now to understand how inflammation in the body affects the brain, and it looks like this may be via the glial cells.
Thank you!
Many thanks to the lab team and the funders who make it possible including the Alzheimer’s Society, European Research Council, Alzheimer’s Research UK, and the UK Dementia Research Institute.
We are optimistic that fundamental research like ours will help develop life-changing treatments for dementias.



