
Dr Jean-Charles Nault
Gastroenterologist and Hepatologist, International Liver Cancer Association

The most widespread form of liver cancer is hepatocellular carcinoma (HCC), a cancer derived from hepatocytes, the main cell of the liver.
HCC is the fifth and ninth most frequently diagnosed cancer in men and women respectively. It represents the fourth leading cause of cancer-related death in the world.
HCC appears mainly in patients with a chronic liver disease, particularly when this liver disease is advanced and causes cirrhosis.
Causes and diagnosis of HCC
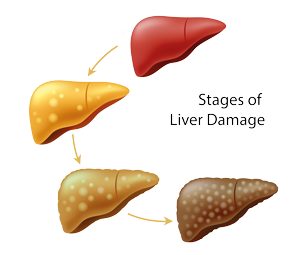
The main causes of liver disease are hepatic virus infection (hepatitis B and C viruses), alcohol abuse and metabolic syndrome (obesity, dyslipidaemia, and diabetes).
The most effective way to prevent the development of HCC is avoiding those agents that are able to damage the liver (universal vaccination against hepatitis B virus, avoiding excessive alcohol consumption, etc.), or treating them before the liver develops cirrhosis.
Surveillance of HCC is recommended in patients with cirrhosis that are at high risk of developing liver cancer. This entails an abdominal ultrasound and blood tests every six months and helps detect small tumours that can be cured.
Unlike most cancers, HCC can often be diagnosed without a biopsy. This is because imaging techniques such as CT scans and MRIs are very accurate indicators that a tumour in the liver is cancerous. If the imaging is inconclusive, a biopsy may be obtained to confirm the diagnosis.
Treatments of HCC
The application of different treatment options will depend on the tumour stage of the patient and liver function.
Liver resection, transplantation and percutaneous ablation (using high temperatures from radiofrequency or microwaves to destroy liver cancer cells) are curative treatments of HCC.
Nonsurgical therapies such as transarterial chemoembolisation may be recommended to shrink the tumour or prevent further growth. This allows a mixture of chemotherapy and embolic agent to be delivered directly to the tumour through blood vessels, which effectively blocks the blood supply to the tumour.
Finally, recent advances have been made in treatments of HCC that are not amenable to curative therapies or not accessible to transarterial chemoembolisation. Several drugs are currently available and act as cancer growth blockers, while several clinical trials testing new drugs are ongoing, with recent data suggesting the potential benefit of immunotherapy to patients with HCC.


